Understanding Mental Health & Wellness
Do I Have An Issue?
This can be a difficult question to answer. All of us experience difficult times. But consistently experiencing some of the following symptoms may be a sign that you’re struggling.
Am I burnt out?
Feeling emotionally, physically, and mentally exhausted and caring less about your clients and patients could indicate that you are burnt out.
Feeling like an imposter?
Imposter syndrome is the feeling of self-doubt. It relates to you feeling like you don’t belong, that you don’t know what you are doing, or that you only got this far by “faking it”.
Am I experiencing compassion fatigue/empathic stress?
Stress we feel as caregivers when we see our clients and patients experience pain, distress, and grief leads to compassion fatigue, or empathic distress. Those experiencing this form of stress often exhibit:
- Dissociation
- Numbness
- Social isolation
- Hypervigilance
- Sleep problems
- Fearfulness
- Avoidance of, or obsession with, the traumatic incident
It’s important to understand that everyone processes these challenges differently. Let’s look at things a little deeper below.
Why Do I Feel This Way?
A lot of terms are used when we talk about the issues surrounding mental health and wellness. Understanding some of the language, symptoms, and situations surrounding mental health and wellness can help you understand where you’re at. Let’s unpack a few of the most common ones, so we’re all on the same page.
Choose from the terms above to jump to the term(s) of interest, or scroll down to explore on your own.
Mental Health & Wellness
What Do We Mean When We Refer to Mental Health?
Mental health describes our thoughts, emotions, and reactions to the world around us, both physical and behavioural. We call these characteristics the four dimensions of mental health and wellbeing.
Mental health has come to be associated with mental disorders and illness, but it is not just the absence of serious mental illness. The term itself actually describes the state of psychological wellbeing.
Similar to physical health, mental illness can be managed and treated to reduce impact on an individual’s quality of life. On the other hand, someone with poor mental health may not always have a specific disorder or illness; mental health is impacted by the stress of balancing work, life, and relationships. Fortunately, you can build up your mental health and well-being to buffer against stress and poor mental health.
For more information:
Wellness
-
Emotional
Coping effectively with life and creating satisfying relationships
-
Financial
Satisfaction with current and future financial situations
-
Social
Developing a sense of connection, belonging, and a well-developed support system
-
Spiritual
Expanding a sense of purpose and meaning in life
-
Occupational
Personal satisfaction and enrichment from one’s work
-
Physical
Recognizing the need for physical activity, healthy foods, and sleep
-
Intellectual
Recognizing creative abilities and finding ways to expand knowledge and skills
-
Environmental
Good health by occupying pleasant, stimulating environments that support well-being
Hover over each segment to reveal the 8 different dimensions of wellness.
Should I Consider Myself “Well”?
Wellness refers to a positive state of mental health and wellbeing. Being “well” does not mean being happy all the time. It’s not about having only good days. It means you are able to cope with the bad days, that you feel emotionally balanced overall, and that you are generally content with yourself, the world, and your life.
Did You Know?
Mental and emotional wellness are important aspects of overall wellness, which can be broken out into 8 different dimensions.
In 2018, the OVMA asked veterinarians to participate in a survey to help identify sources of stress and anxiety amongst members. The two biggest sources of stress that were identified were finances (Financial) and work/life balance (Occupational).
Mental Illness
How Does Mental Illness Differ from Wellness?
Mental illness is a broad term that describes a wide range of disorders that affect mood, thinking, and behaviour, such as:

Mood disorders
Eating disorders
Personality disorders
Schizophrenia
Anxiety disorders

Substance use disorders
Mental illness refers to a prolonged, negative state of mental health and wellbeing that impacts your ability to function in your day-to-day life. Mental illness often has physical consequences on energy levels, appetite, sleep. Mental illness can also impact your ability to think clearly and make decisions.
Causes are often complex and may include genetics, demographics, life history, stressful events, and environmental influences. It may be treated or managed to reduce the impacts it may have on an individual’s quality of life.
According to the Canadian Mental Health Association, 1 in 2 Canadians will experience a mental illness by the age of 40.
Why the Stigma Around Mental Health & Wellness?
Despite the overwhelming number of Canadians who experience mental illness in their lifetime, stigma is very common. This is often due to the fear and discomfort that many people experience when discussing mental health and illness.
Stigma refers to:
- Negative stereotypes of those with mental illness
- Media portrayals of individuals with mental illness as unstable, dangerous, and unpredictable
This stigma leads us to:
- Avoid discussion about mental health and illness
- Discriminate against those with mental illness
- Trivialize, belittle, or patronize those with mental illness
Are There Challenges Unique to Veterinarians?
The most common mental illnesses veterinarians experience are mood disorders and substance abuse.
These illnesses can be triggered by:
- Occupational stressors
- Traumatic experiences
- Burnout
- Compassion fatigue/empathic distress
What Are the Most Common Stressors?
Age
Younger veterinarians are reported to be at highest risk for Burnout, a state of mental exhaustion, and other negative mental health outcomes1. Early career veterinarians are also the most likely to experience Imposter Syndrome, where they feel unprepared for the demands and challenges of the profession.
Gender
Female veterinarians are also reported to be at high risk for Burnout and other negative mental health outcomes1.
Home life
Among many other things, new parents may find they struggle more with work-life balance.
Business life
Practice owners may find it challenging to promote a positive and engaged team culture. This adds a lot of stress to an already stressful profession. On the other hand, sole practitioners may suffer from professional and social isolation2.
Veterinarian Stories
- Dark Shadows: Drug Use and Addiction in the Veterinary Workplace
- Stressed, Depressed Veterinarians Fall Prey to Addiction
- Drug Diversion and Veterinarians

Interested in a veterinarian’s perspective on this topic?
Check out this podcast featuring Dr. Carrie Jurney.
References
- CVMA News. 2012. “Wellness of Veterinarians: CVMA National Survey Results.” Canadian Veterinary Journal 53: 1159–60.
- Bartram, David J., and David S. Baldwin. 2010. “Veterinary Surgeons and Suicide: A Structured Review of Possible Influences on Increased Risk.” Veterinary Record 166 (13): 388–97. https://doi.org/10.1136/vr.b4794.
Do I Have a Mood Disorder? Depression & Anxiety
Feelings of sadness and anxiety can be a normal part of the ups and downs of day-to-day life. They can also be a normal response to stress. However, prolonged feelings, extreme feelings, or those which impact your ability to function normally might indicate a disorder that requires treatment.
What Can You Do About It?
Seek counselling
Talking to a professional can help you understand the relationships between the way you think, feel, and act.
Reach out
Don’t let your relationships suffer. Once you understand the way you think, act, and feel, focus on how that impacts your relationships and how you interact with people.
Manage your time to prioritize yourself
Eating, sleeping, and regular exercise are important to keep you physically healthy and are important for buffering yourself to the effects of stress.
For more information:
- Your doctor can be an excellent resource for diagnosis and referral to counsellors or therapists in your area
- Canadian Mental Health Association
- Mood Disorders Association of Ontario


Substance Abuse
Substance abuse is a pattern of harmful or hazardous use of psychoactive substances, including alcohol and illicit drugs.This is oftentimes associated with underlying and/or accompanying health and psychiatric problems.
It’s important to know that you can receive treatment for substance abuse issues without losing your license.
Speak with your healthcare provider if you feel that you need help overcoming a substance abuse issue. They can help connect you with appropriate resources and support in your area.
For more information:
What Does it Mean to Be Resilient?
Resilience describes an individual’s ability to cope with, or recover from, stress and stressful events. It’s the capacity to positively adjust to adversity. Most importantly, resilience is a pattern of thoughts and actions that can be learned by anyone1.
What Does the Research Say?
Resilience can buffer you against occupational stressors such as burnout and compassion fatigue/empathic distress2. An individual’s resilience is influenced by both their physical and mental health3.
Four Strategies to Build Resilience
- Physical resilience = mental resilience! Physical activity is associated with resilience to occupational stress in healthcare professionals6. This could include spending some time in nature — go for a hike or just take your lunch break outdoors8.
- You are what you eat. Focus on nutrition7 and check in with your general practitioner if you have a history of, or suspect you may have, any nutritional deficiencies. Make time to eat during the workday.
- Sleep your way to wellness. Get enough quality sleep, and seek professional help if you aren’t able to sleep well. Sleep disturbances have been associated with depression, anxiety, and burnout9,10.
- Make social connections. This could be socializing at or outside work, or talking with someone (coworker, boss, friend, family member) directly about what you’re feeling. Supportive relationships and personal resources provide a wealth of mental health benefits5.

Check out our I Matter section for more on resilience.
References
- American Psychological Association. The Road to Resilience. https://www.apa.org/helpcenter/road-resilience
- Cake, Martin A., Michelle M. McArthur, Susan M. Matthew, and Caroline F. Mansfield. 2017. “Finding the Balance: Uncovering Resilience in the Veterinary Literature.” Journal of Veterinary Medical Education 44 (1): 95–105. https://doi.org/10.3138/jvme.0116-025R
- Walsh, Roger. 2011. “Lifestyle and Mental Health.” American Psychologist 66 (7): 579–92. https://doi.org/10.1037/a0021769
- Fox, Susan, Sinéad Lydon, Dara Byrne, Caoimhe Madden, Fergal Connolly, and Paul O’Connor. 2018. “A Systematic Review of Interventions to Foster Physician Resilience.” Postgraduate Medical Journal. https://doi.org/10.1136/postgradmedj-2017-135212
- Mastenbroek, Nicole J J M. 2017. “The Art of Staying Engaged: The Role of Personal Resources in the Mental Well- Being of Young Veterinary Professionals.” Journal of Veterinary Medical Education 44 (1): 84–94. https://doi.org/10.3138/jvme.0216-041R1
- Gerber, Markus, Ingibjörg H. Jonsdottir, Magnus Lindwall, and Gunnar Ahlborg. 2014. “Physical Activity in Employees with Differing Occupational Stress and Mental Health Profiles: A Latent Profile Analysis.” Psychology of Sport and Exercise 15 (6): 649–58. https://doi.org/10.1016/j.psychsport.2014.07.012
- Walsh, Roger. 2011. “Lifestyle and Mental Health.” American Psychologist 66 (7): 579–92. https://doi.org/10.1037/a0021769
- Wolf, Megan R., and Jason B. Rosenstock. 2017. “Inadequate Sleep and Exercise Associated with Burnout and Depression among Medical Students.” Academic Psychiatry 41 (2): 174–79. https://doi.org/10.1007/s40596-016-0526-y
- Alvaro, Pasquale K., Rachel M. Roberts, and Jodie K. Harris. 2013. “A Systematic Review Assessing Bidirectionality between Sleep Disturbances, Anxiety, and Depression.” Sleep 36 (7): 1059–68. https://doi.org/10.5665/sleep.2810
- Swensen S, Kabcenell A, Shanafelt T. Physician-Organization Collaboration Reduces Physician Burnout and Promotes Engagement: The Mayo Clinic Experience. J Healthc Manag. 2016 Mar-Apr;61(2):105-27.
What Does It Mean to Be Burnt Out?
Burnout is a state of emotional, physical, and mental exhaustion caused by prolonged stress. It can lead to caring less about your clients and patients than you used to, having negative feelings toward them, or distancing yourselves from them (depersonalization)1.
Common in Medical Professions
Burnout can happen in any job, but it is especially common in medical professions. Over ⅓ of surveyed Canadian veterinarians were experiencing burnout in 20172.
Burnout occurs when job demands exceed job rewards & resources:
Demands include:
- Working long hours without rest3
- Excessive patient load3
- Janitorial work3, such as mopping floors and cleaning up bodily fluids
- Dealing with difficult clients and patients
- Dealing with toxic team members4 and/or team culture
Rewards and resources include:
- Support from coworkers and supervisors3
- Breaks and time off
- Satisfaction for doing your job well, helping patients and clients, and building your skills
- Getting paid commensurate to experience levels
- Feeling appreciated for the work you do
What Can You Do About It?
Reach out
Connect with friends and family members and express some of your thoughts on the way you’ve been feeling.
Develop friendships with coworkers
This can help make the work day more enjoyable.
Steer clear of negativity
Avoid coworkers that contribute to negative morale.

Check out our I Matter section for more.
References
- Maslach, Christina, Wilmar B Schaufeli, Michael P Leiter, and W Shaufeli. 2001. “Job Burnout.” Annual Review of Pyschology 52: 397–422. https://doi.org/10.1146/annurev.psych.52.1.397
- Perret, Jennifer L., Colleen O. Best, Jason B. Coe, Amy L. Greer, Deep K. Khosa, and Andria Q. Jones-Bitton. 2019. “Prevalence of Mental Health Outcomes among a Sample of Canadian Veterinarians.” Journal of the American Veterinary Medical Association, (in press).
- Hayes, Galina M., Denise F. LaLonde-Paul, Jennifer L Perret, Andrea Steele, Marina McConkey, William G. Lane, Rosalind J. Kopp, Hannah K. Stone, Andria Jones-Bitton. 2019. “Investigation of burnout syndrome and associations with job-related risk factors in veterinary technicians working in specialty teaching hospital settings: a multi-center cross-sectional study.” Unpublished.
- Moore, Irene C, Jason B Coe, Cindy L Adams, Peter D Conlon, and Jan M Sargeant. 2014. “The Role of Veterinary Team Effectiveness in Job Satisfaction and Burnout in Companion Animal Veterinary Clinics.” Journal of the American Veterinary Medical Association 245 (5): 513–24. https://doi.org/10.2460/javma.245.5.513
- Black, Anne F, Helen R Winefield, and Anna Chur-Hansen. 2011. “Occupational Stress in Veterinary Nurses: Roles of the Work Environment and Own Companion Animal.” Anthrozoos 24 (2): 191–202. https://doi.org/10.2752/175303711X12998632257503
Am I Experiencing Compassion Fatigue/Empathic Distress?
Compassion fatigue is caused by:
- Burnout
- Empathy
- Witnessing the pain, trauma, or grief of others
- Attachment to your pets4
- Ethical conflict5,6
- Feeling alone in your concern
Some of the key symptoms include7:
- Dissociation, which is similar to depersonalization in burnout
- Numbness
- Social isolation
- Hypervigilance
- Sleep problems
- Fearfulness
- Avoidance of, or obsession with, the traumatic incident
Recently, some experts have moved away from the term “compassion fatigue,” and suggested that compassion may be the solution, rather than the problem9. Empathic distress is one of the newer terms being used9. Empathy means feeling the distress of others, which can be extremely tiring, and lead to exhaustion, avoidance, and even anger toward patients and clients.
Empathic stress has been described as a combination of burnout and secondary traumatic stress1. Secondary Traumatic Stress describes the stress we feel as caregivers when we see our clients and patients experience pain, distress, and grief. This condition is specific to caregiving work, such as veterinarians, veterinary technicians, physicians, nurses, psychologists, and social workers.
Veterinarians Are At Risk
A 2019 survey highlighted that Canadian veterinarians were experiencing secondary traumatic stress at very high levels2. A recent systematic review found vets to be in the top 3 professions for experiencing secondary traumatic stress3.
Unlike burnout, satisfaction with your job may still be high. This has been called “the paradox of compassionate work8” or “the double-edged sword of human empathy”9. The very same experiences that bring fulfillment, such as connecting with clients and patients, can also be draining. Compassion satisfaction leads many medical professionals to work harder and push themselves further toward burnout or compassion fatigue. The “cost of caring”10 may be unavoidable at times, but it can be managed without sacrificing client and patient care.
What Can You Do About It?
Spend time alone
Practicing mindfulness and meditation can help you to understand the way that you feel.
Re-energize yourself
You don’t feel well when you don’t eat, sleep, or exercise well.
Connect with others
Engage in meaningful conversation. Reconnect with your family and friends.
Interested in an Ontario veterinarian’s perspective on this topic?
Check out this podcast featuring Dr. Jennifer Perret.
Check out our I Matter section for more.
References
- Stamm, Beth Hudnall. 2010. The Concise ProQOL Manual. 2nd Edition. Pocatello.
- Perret, Jennifer L., Colleen O. Best, Jason B. Coe, Amy L. Greer, Deep K. Khosa, and Andria Q. Jones-Bitton. 2019. “Prevalence of Mental Health Outcomes among a Sample of Canadian Veterinarians.” Journal of the American Veterinary Medical Association, (in press).
- La Rosa, GM De, JA Webb-Murphy, SF Fesperman, and SL Johnston. 2018. “Professional Quality of Life Normative Benchmarks.” Psychological Trauma: Theory, Research, Practice, and Policy 10 (2): 225–28. https://doi.org/10.1037/tra0000263
- Black, Anne F, Helen R Winefield, and Anna Chur-Hansen. 2011. “Occupational Stress in Veterinary Nurses: Roles of the Work Environment and Own Companion Animal.” Anthrozoos 24 (2): 191–202. https://doi.org/10.2752/175303711X12998632257503
- Moses, Lisa, Monica J. Malowney, and Jon Wesley Boyd. 2018. “Ethical Conflict and Moral Distress in Veterinary Practice: A Survey of North American Veterinarians.” Journal of Veterinary Internal Medicine 32 (6): 2115–22. https://doi.org/10.1111/jvim.15315
- Rollin, Bernard E. 2011. “Euthanasia, Moral Stress, and Chronic Illness in Veterinary Medicine.” Veterinary Clinics of North America – Small Animal Practice. Elsevier Ltd. https://doi.org/10.1016/j.cvsm.2011.03.005
- Cohen, Susan P. 2007. “Compassion Fatigue and the Veterinary Health Team.” Veterinary Clinics of North America – Small Animal Practice. Elsevier Inc. https://doi.org/10.1016/j.cvsm.2006.09.006
- Polachek, Alicia J., and Jean E. Wallace. 2018. “The Paradox of Compassionate Work: A Mixed-Methods Study of Satisfying and Fatiguing Experiences of Animal Health Care Providers.” Anxiety, Stress and Coping 31 (2): 228–43. https://doi.org/10.1080/10615806.2017.1392224
- Russell, Mark, and Matt Brickell. 2015. “The ‘Double-Edge Sword’ of Human Empathy: A Unifying Neurobehavioral Theory of Compassion Stress Injury.” Social Sciences 4 (November): 1087–1117. https://doi.org/10.3390/socsci4041087
- Sinclair, Shane, Shelley Raffin-Bouchal, Lorraine Venturato, Jane Mijovic-Kondejewski, and Lorraine Smith-MacDonald. 2017. “Compassion Fatigue: A Meta-Narrative Review of the Healthcare Literature.” International Journal of Nursing Studies 69 (April): 9–24. https://doi.org/10.1016/j.ijnurstu.2017.01.003

How Does Imposter Syndrome Affect You?
Imposter syndrome is self-doubt that relates to feeling like you don’t belong, that you don’t know what you are doing, you aren’t good enough, or that you only got this far by “faking it”.
Imposter syndrome is very common, especially in recent graduates.
Veterinarians Are At Risk
Veterinarians possess certain characteristics that predispose them to question their abilities. For example, many of us have a “perfectionist personality”, which drives us to feel we could always do better. Also consider the fact that years of schooling may have provided concrete evaluation of our skills and comparison with our peers. Yet, when in practice, this type of evaluation is rarely provided.
The veterinary profession also presents a number of situations that cause you to rethink your abilities:
- Veterinarians often work alone or with few peers, which makes it difficult to ascertain how you “compare”.
- Medicine provides ample opportunities for failure, even when we do everything “right”.
- Clients who are grieving or distressed may provide negative feedback via social media.
What Can You Do About It?
Seek a mentor
Engage with experienced veterinarians who can help support you while you build confidence. Bounce ideas off them, and ask for their advice.
Acknowledge what you know
Try being a mentor yourself to a new graduate or student veterinarian. This will build confidence and reassure you that you are indeed skilled and knowledgeable.
Talk about it
Talking about appointments, surgeries, or farm calls that went well or didn’t go well openly can open up dialogue about teachable moments, knowledge or experience gaps, and potentially even clinic protocols or training that needs improvement.
Interested in an Ontario veterinarian’s perspective on this topic?
Check out this podcast featuring Dr. Peter Conlon
Watch this great TED Talk on imposter syndrome:
What is imposter syndrome and how can you combat it?
Easy reads for vets
Am I Setting Unrealistic or Unattainable Goals for Myself?
Setting elevated personal standards and expectations is often motivational for high-achieving individuals. These individuals strive for success, but not everyone accepts that disappointment, mistakes, and failures are par for the course. Without proper expectations, this high-achieving mindset can become toxic where anything less than perfection is acceptable.
Oftentimes, the expectations of perfection can cause anxiety, frustration, and depression1. Perfectionism can cause individuals to be critical of themselves as well as others, and they often have an overwhelming fear of failure, disapproval, or disappointment.
A perfectionist mindset often includes:
- Black and white thinking, where unless something is perfect, it is not good enough.
- Catastrophic thinking, where the thought of making an error will cause your employer/coworker/client to disapprove of you.
- Probability overestimation, or the idea that you can predict your own failure, and expect people to judge or criticize you.
- “I should” statements, where you can agonize over things that have gone wrong, instead of the things that have gone right.
What Can You Do About It?
Change the way you think
Replace self-criticism with statements that focus on accepting that it is impossible to control every outcome of every situation. Practice these statements regularly. Tell yourself, “‘I am confident that I gave it my best, and that’s all I can do”.
Take a look at yourself from another’s perspective
It can be difficult to see things from a different point of view. It’s important to consider how others may perceive you. For example, if you decide to take a short break, or time for yourself, ask yourself:
- How might someone else perceive this? Would I be critical of someone else for taking time for themselves?
- Is doing something small for yourself unreasonable?
- What would you recommend to someone feeling the same way you do? — You’d probably recommend they take time for themselves!
Compromise
Be more flexible with the expectations you have of yourself. It is impossible to always say and do the right thing, and you cannot expect to please everyone. With that in mind, what imperfections are you willing to accept? It can provoke anxiety to allow yourself to make an error, so start with some minor things and build from there.
Remember
Having flexible standards does not mean having NO standards. Being realistic about what you can do will motivate you, rather than be held back by the fear of failure. This will allow you to focus on achieving goals and build self-confidence.

References
- Anxiety Canada.How to Overcome Perfectionism. www.anxietycanada.com
Focusing In On Wellness
Mental wellness influences much more than just how you feel day to day. It affects the way you think, your relationships, how you deal with stress, and how you handle the challenges of everyday life. The good news is, you can take steps to control and improve your mental wellness. Mental wellness helps you to:

Be resilient
Being able to deal with stress, being able to bounce back from adversity.

Build self-confidence
Recognize that you are good at many things, be confident in your strengths, and appreciate that no one is perfect — find ways to constructively work on your weaknesses.
Be flexible
Find ways to adapt to new and unexpected changes in our personal and professional lives.
What Are the Impacts of Wellness?
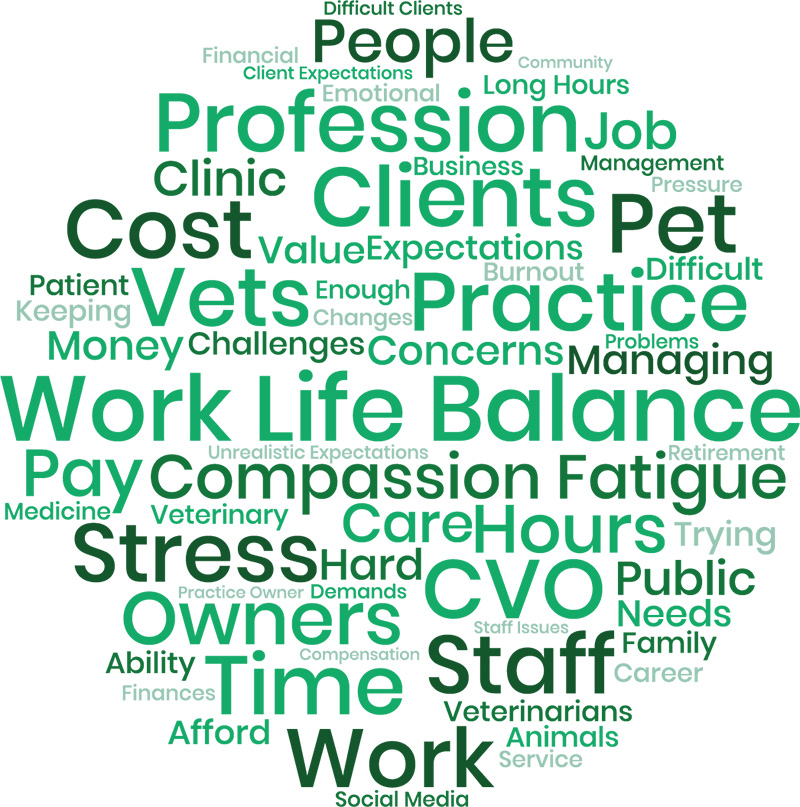
You can be experiencing mental health issues and still be functioning at a high level. However, mental health issues and poor mental wellness contribute to a number of negative outcomes for individuals and the workplace. The word cloud below demonstrates some of the terms Ontario veterinarians used to describe their wellness challenges.
Impacts On Veterinarians
Veterinarians are a high risk group for occupational stress and poor mental health. In a 2018 study, 62% of OVMA members reported they are experiencing stress and anxiety. What’s more, surveyed Canadian veterinarians in 2017 had similar levels of burnout to other medical professions, but much higher levels of secondary traumatic stress1; among the highest in all medical and caregiving professions2.
Medical professionals are notorious for being reluctant to recognize and treat their own mental health disorders, and veterinarians are no exception4. Poor mental health is a contributing factor to the relatively high level of death by suicide that has been well-recognized in the profession5.
Moral and ethical stress can be caused by the nature of the veterinarian-client-patient relationship; for example, when there is a discrepancy between the client’s desires and the patient’s needs3. This presents a challenge for the empathetic veterinarian.
A groundbreaking study led by CDC researcher Dr. Randy Nett reports that nearly one in 10 veterinarians in the United States may suffer from serious psychological distress and more than one in six may have experienced suicidal ideation since graduation9.
Impacts on Veterinary Practices
The mental health of the veterinary team greatly impacts your practice and the quality of care provided to clients and patients. Client satisfaction and communication are major drivers of clinic profit.
Business impacts of burnout include:
- Increased staff turnover7
- High number of sick leave/sick days
- Reduced staff productivity
- Poor client communication
- Reduced client satisfaction
- Reduced level of patient care8
-
1Increased staff turnover7
-
2High number of sick leave/sick days
-
3Reduced staff productivity
-
4Poor client communication
-
5Reduced client satisfaction
-
6Reduced level of patient care8
References
- Perret, Jennifer L., Colleen O. Best, Jason B. Coe, Amy L. Greer, Deep K. Khosa, and Andria Q. Jones-Bitton. 2019. “Prevalence of Mental Health Outcomes among a Sample of Canadian Veterinarians.” Journal of the American Veterinary Medical Association, (in press).
- La Rosa, GM De, JA Webb-Murphy, SF Fesperman, and SL Johnston. 2018. “Professional Quality of Life Normative Benchmarks.” Psychological Trauma: Theory, Research, Practice, and Policy 10 (2): 225–28. https://doi.org/10.1037/tra0000263
- Moses, Lisa, Monica J. Malowney, and Jon Wesley Boyd. 2018. “Ethical Conflict and Moral Distress in Veterinary Practice: A Survey of North American Veterinarians.” Journal of Veterinary Internal Medicine 32 (6): 2115–22. https://doi.org/10.1111/jvim.15315
- Skipper, Gregory E., and Jerome B. Williams. 2012. “Failure to Acknowledge High Suicide Risk among Veterinarians.” Journal of Veterinary Medical Education 39 (1): 79–82. https://doi.org/10.3138/jvme.0311.034R
- Fink-Miller, Erin L, and Lisa M Nestler. 2018. “Suicide in Physicians and Veterinarians: Risk Factors and Theories.” Current Opinion in Psychology. https://doi.org/10.1016/j.copsyc.2017.07.019
- Cron, William L, John V Slocum, David B Goodnight, and John O Volk. 1998. “JAVMA Executive Summary: Impact of Management Practices and Business Behaviors on Small Animal Veterinarians’ Incomes.” Journal of the American Veterinary Medical Association 215: 161–83.
- Moore, Irene C, Jason B Coe, Cindy L Adams, Peter D Conlon, and Jan M Sargeant. 2014. “The Role of Veterinary Team Effectiveness in Job Satisfaction and Burnout in Companion Animal Veterinary Clinics.” Journal of the American Veterinary Medical Association 245 (5): 513–24. https://doi.org/10.2460/javma.245.5.513
- Ruby, Kathleen L., and Richard M. DeBowes. 2007. “The Veterinary Health Care Team: Going from Good to Great.” Veterinary Clinics of North America – Small Animal Practice. Elsevier Inc. https://doi.org/10.1016/j.cvsm.2006.10.004
Where Do We Go From Here?
Supporting wellness is good for you, your associates, and your practice. Each of the following content sections provide strategies to build resiliency.